We were thrilled to participate in HLTH 2022 and want to thank everyone who took the time to connect with us—whether stopping by our booth, scheduling a demo with our team, or attending one of our Bourbon receptions.
We were inspired to hear from so many healthcare leaders about the new approaches they’re taking to combat rising costs and accelerate the shift to value.
Here are 3 takeaways from an incredible event:
Employers are taking on rising healthcare costs through new benefits strategies…
The conference took place against a backdrop of increasing uncertainty for employers—from the lingering effects of the pandemic and the “Great Resignation” to rising interest rates and recession fears.
One thing that’s become extremely predictable for employers is ever-rising healthcare costs, often without a corresponding boost in outcomes.
At the conference, we spoke with HR and benefits leaders who are determined to change this.
In the past, their companies managed healthcare costs by pursuing the best discounts and widest networks with their health plan partners. They’re now looking to take a more proactive role in designing an overall benefits package to better meet the unique health and wellness needs of their employee populations.
This means enhancing their benefits offerings with point solution programs designed to boost health outcomes while reducing the total cost of care.
…but these employers need a way to cut through the noise
Employers seeking to take a more proactive role in selecting point solution programs face a problem: They’re being bombarded with pitches from solution vendors and aren’t sure how to truly determine which programs are going to minimize costs while improving employee health.
The HR and benefits leaders we spoke to listed a number of questions they’re trying to answer, including:
- Should they invest in diabetes management, heart health, fitness tracking, clinical outreach, mental health services, or an array of other choices?
- How can they get employees and their families to engage with each program to its fullest potential?
- How can they measure the success of these programs?
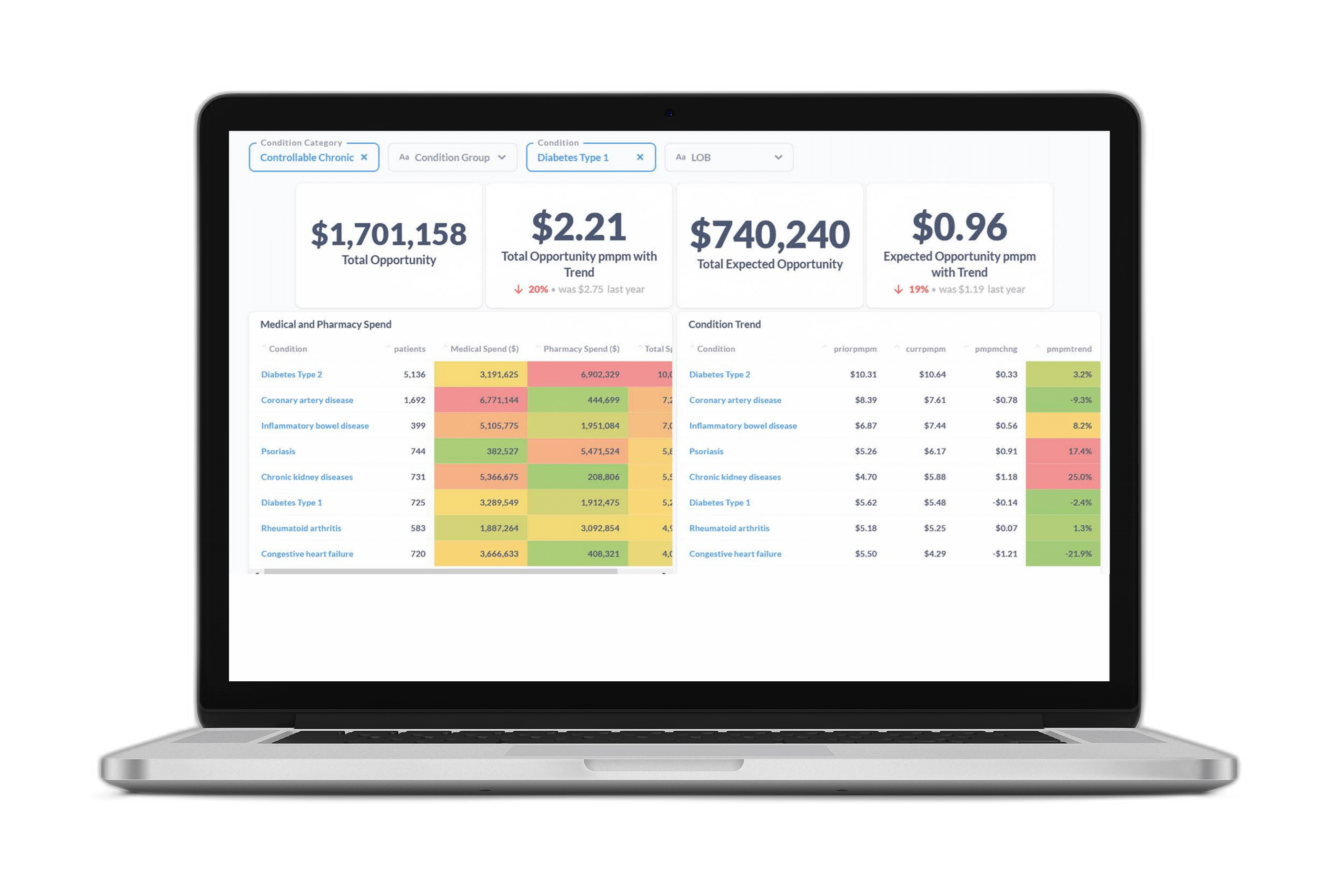
Answering these questions requires a data-backed approach to understand the specific needs of an employer population and quantify the impact of new and existing programs. At Certilytics, we help customers answer these questions using our Impact Evaluator, which equips HR and benefits teams with hard numbers showing which point solutions are the right fit to achieve their goals.
Case Study: Learn how we helped one HR and benefits team choose the right point solution programs and measure results.
For solution providers, this means you need to demonstrate ROI
The past few years have seen an explosion in the number of digital health and wellness solutions designed to boost health and well-being while reducing costs.
This was on full display at the conference, with hundreds of exhibitors showcasing their new disease management programs, engagement strategies, fitness trackers, mindfulness apps, and more.
The question for solution providers is how to stand out in such a crowded marketplace.
The answer: They need hard numbers demonstrating ROI and showing that their solutions will make a substantial, positive impact on health outcomes and cost.
At the conference, HR and benefits leaders told us they’re looking for programs that can demonstrate real, quantifiable impacts to give them confidence that a new solution or tool will have real value for employees and their families.
Thanks again to all those who made time to connect with us in Las Vegas—we hope to see you again (or for the first time) at next year’s conference!
To learn more about how Certilytics can help you accelerate the shift to value, contact us to schedule a meeting with our team.