With the passing of the Consolidated Appropriations Act of 2021, employers were given a lot more responsibility over the healthcare services they purchase for their employees and their families.
While these regulations made headlines, not much has been said on how exactly employers can be sure they’re serving as the best steward of their health and benefit offerings.
So, how can you be confident you’re giving the best recommendations to your clients so their healthcare services are as efficient and affordable as they can be? What does success in this role look like?
The good news is we can help you. We’re partnering with benefit advisors to find these answers in their client’s data so they can quickly and effectively craft strategies that enable their clients to not just comply with the regulations, but turn this responsibility into an opportunity to better meet the needs of their employees and their families.
Here are three essential things you must have from your data and analytics partners in order to turn your client’s compliance into opportunity:
1. Find a Data Partner to Help Unify and Enrich Your Client’s Data with Predictive Analytics
To ensure your benefit recommendations are in the best interest of your client’s employee population, you must first understand their employees’ existing and emerging needs.
This understanding begins with a complete picture of the employees’ and their families’ overall health.
This can certainly be a challenge given all of the data from an employers’ health partners and program solution vendors. Especially since most employers haven’t traditionally been in the business of collecting data beyond medical and pharmacy claims.
So what’s the best way to connect the data?
This is where a data partner comes in. You’ll need your partner to not only collect the data from all these different sources, but link it all together.
By doing this, you can be confident that your benefit recommendations have come from a single, precise source of truth.
How can predictive analytics be a game-changer?
Connected data will help your clients meet their fiduciary responsibilities, but enhancing that data with predictive analytics will help them succeed. If the data analysis only tells you what has happened in the past, you can’t make the best benefit recommendations for your client’s health benefits plan now and in the future.
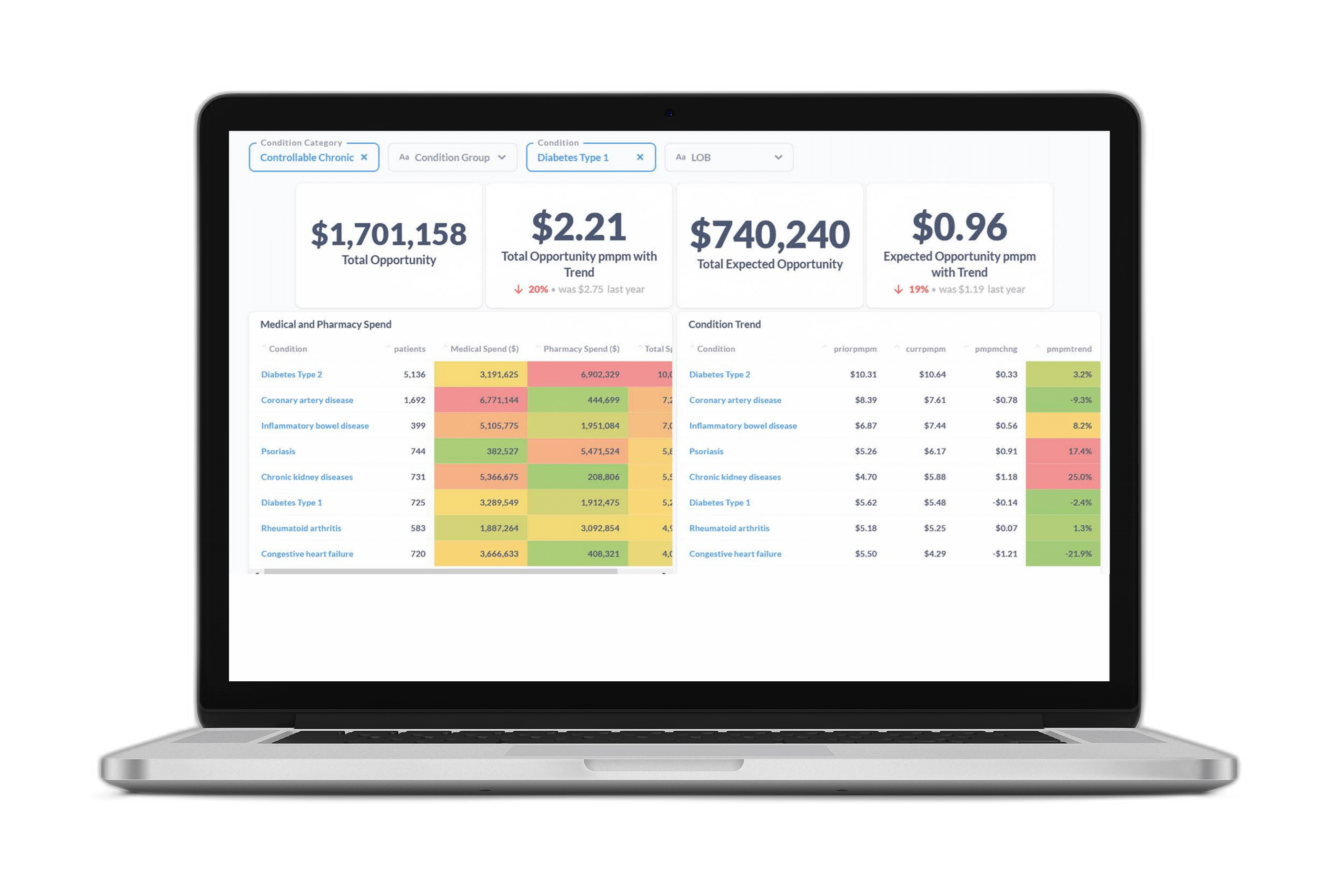
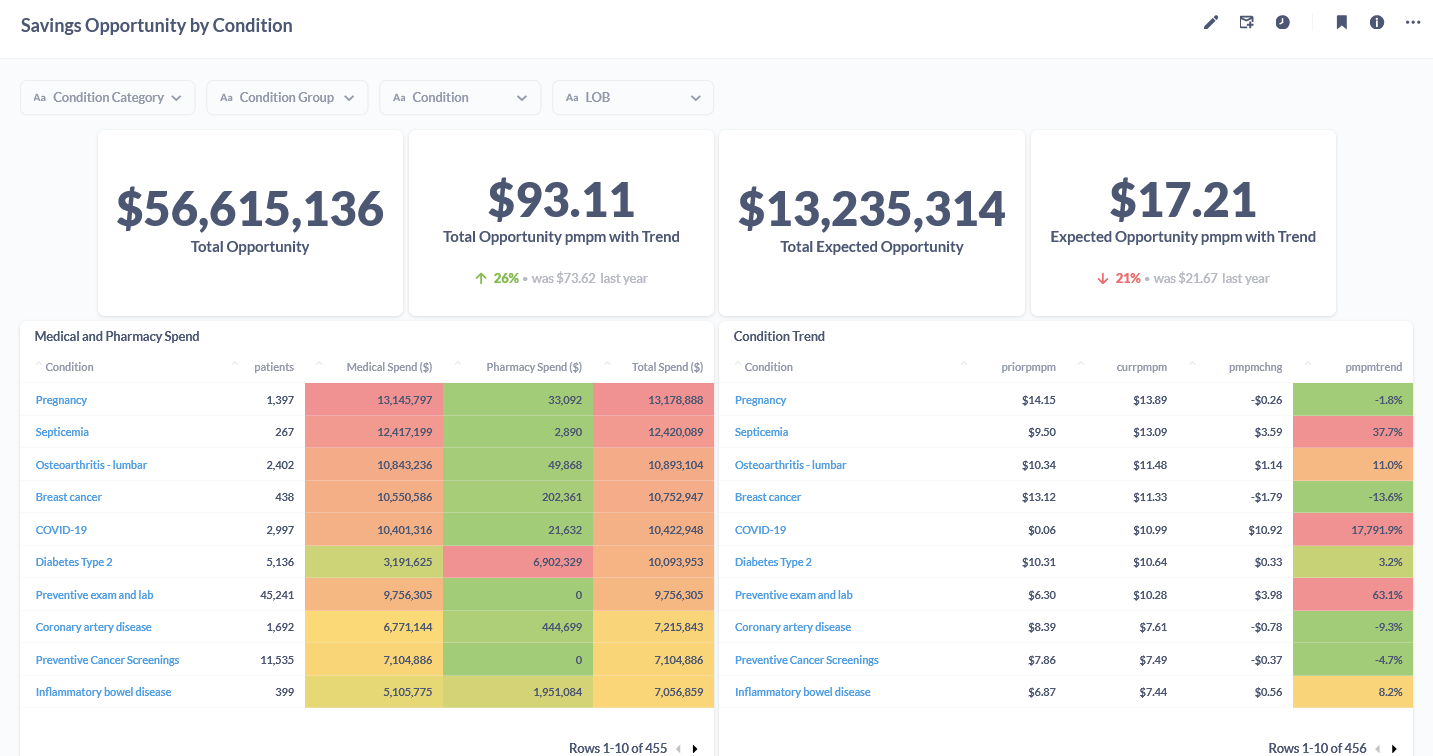
A predictive analytics partner enables you to look forward and identify emerging trends and health risks within your client’s employee population. For example, below is a snap shot of what our customers see when they leverage our predictive analytics solutions. They can identify the highest areas of spend, which is the first step in implementing programs and strategies to proactively minimize those costs and keep their employees healthier.
2. Use Your Client’s Data to Identify the Largest Opportunities for Cost Savings and Improved Health Outcomes
Once your team understands the risks and needs in the employer’s population, you can begin exploring the most effective ways to keep their employees and their families healthy.
The key is knowing the best ways to reach them. This insight is the difference between just identifying risk and actually improving health outcomes. It’s also integral to not just pinpointing high costs, but addressing avoidable spending.
How do you know who will respond to point solution vendors’ efforts? How do you know which type of outreach methods would generate the most engagement?
A predictive analytics partner should answer these questions for you, allowing you to build recommendations for proactive programs around these individuals.
For example, at Certilytics, we provide our customers with an “Expected Opportunity” score. It is this opportunity that accounts for the likelihood of an employee to engage and change their behavior. With our platform, you can see the likelihood of engagement down to the individual level, enabling you to build program recommendations that match the right employee to the right program at the right time.
3. Leverage Employer Vendor Partners’ Data to Evaluate the Impact of Programs and Strategies on Reducing the Total Cost of Care
Your customer’s data has helped you build program recommendations that will have the greatest impact on health outcomes and costs.
But, how can you be confident you made the right decisions?
You need a data partner who can work with you to collect data from all your client’s solution vendors and evaluate their performance from both a health and cost perspective.
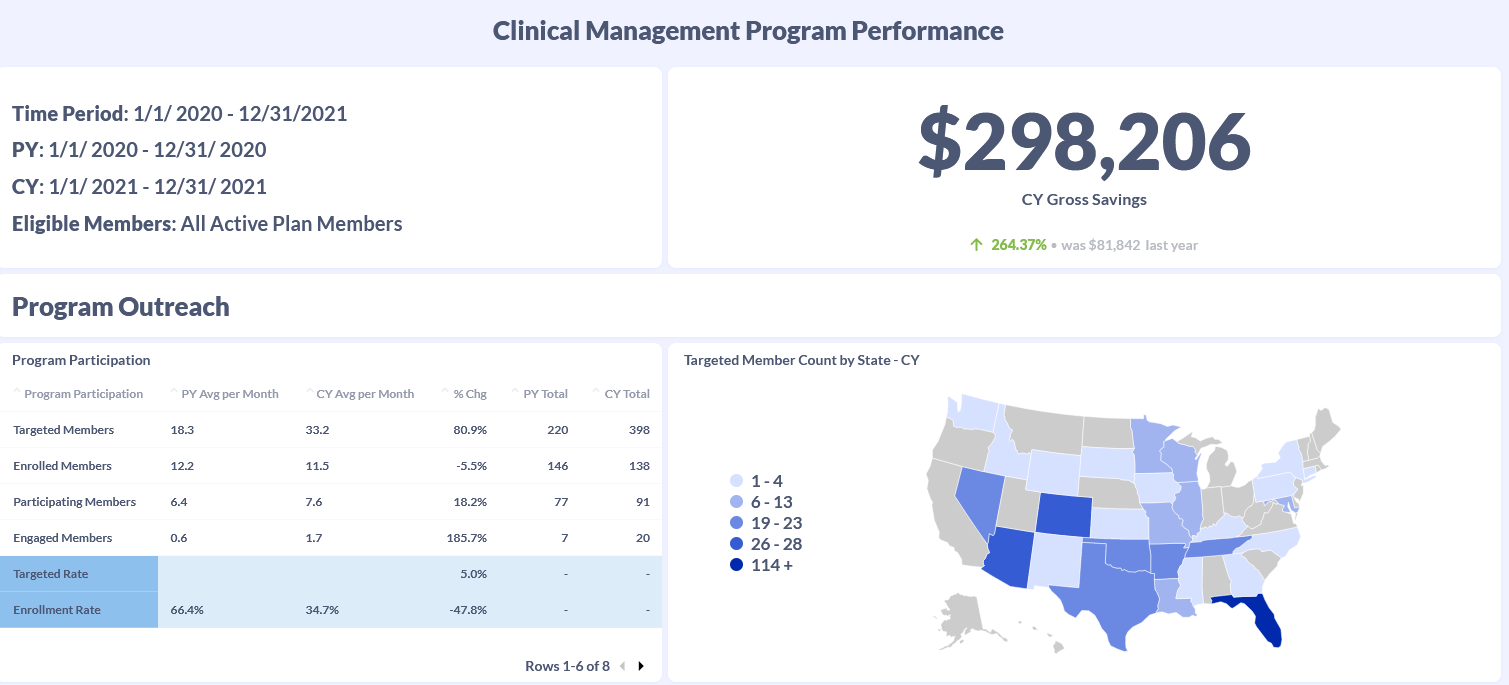
At Certilytics, our predictive insights are helping our customers track the progress of their point solution programs and measure their impact on ROI. With this insight, they assess which programs are most effective at impacting behavior, improving health, and reducing healthcare costs.
Want to learn more about how Certilytics can help you leverage data to make recommendations that enable your employer clients to succeed in their role as health plan fiduciaries?