The past year was anything but normal.
Traditional ideas about care pathways and outreach methods were upended as the pandemic accelerated shifts toward virtual care, digital health and wellness, and reducing social health barriers.
As 2021 comes to a close, we’re reflecting on our conversations and partnerships with some of the nation’s most innovative healthcare organizations – what challenges were overcome, what new priorities surfaced, and what will be the top areas of focus in 2022.
Here are five things we learned this past year that remain top of mind for healthcare leaders:
1. Payers are awash in clinical point solutions—and need a way to connect all the data.
Benefit teams and health plans are investing in an array of clinical point solutions designed to improve health outcomes and boost employee well-being and productivity—all while reducing the total cost of care.
These range from chronic disease management programs to digital lifestyle apps for fitness tracking, sleep improvement, mindfulness, and more.
But payer organizations are struggling to quantify the return on investment from all these point solutions—and looking for ways to optimize these programs to ensure they’re matching the right member with the right programs at the right time.
In response, benefit leaders are replacing legacy data warehousing solutions and instead adopting AI-enabled analytic tools to equip their organizations with easy-to-understand predictive analytics that measure program performance and increase employee engagement. This enables them to improve their benefit offerings, design high-performance networks, and incentive their health partners to focus on value, not fee-for-service.
2. Social Determinants of Health (SDoH) is more than a buzzword.
For years, healthcare leaders have been talking about health equity and the Social Determinants of Health (SDOH). But these concepts have often felt like buzzwords, with few ideas for how to respond to the growing understanding that factors outside a clinician’s control have a major impact on health.
Now, healthcare leaders are looking for ways to translate SDOH insights into real-world impact.
At Certilytics, we recently released an AI-powered model that predicts each member’s SDOH risk, enabling interventions at both the member and population levels to improve healthcare access and outcomes with cost and efficiency measures.
This model is designed to help health plans, employers, and provider health systems gain deeper insights into member behaviors and develop new strategies, programs, and partnerships to address social health barriers.
3. The pandemic is powering a digital health revolution.
The COVID-19 pandemic has brought digital health to the forefront—and there’s no turning back.
But the shift to digital health will only be effective if guided by data-backed decision-making. This will require strategic investments in analytics that support reaching the right members at the right time via the right form of outreach—a key capability we help our clients achieve through our Forecasts risk stratification tool.
The pandemic is also accelerating the shift toward virtual care and telehealth, which will require investment in AI capabilities that ensure individual patients are matched with the right services and care settings. That’s why Certilytics built a predictive model that determines a patient’s likelihood of utilizing telehealth services—enabling our clients to target their virtual care programs more effectively.
4. Specialty Rx costs are a major concern.
Plan sponsors are seeing more and more of their total pharmacy spend being attributed to specialty drugs. Evernorth’s 2020 Drug Trend Report found that just 2% of the company’s covered population used specialty drugs—but this accounted for over half of total spend under the pharmacy benefit.
For anyone interested in practical steps you can take to rein in specialty drug spending, Certilytics is offering a free e-book on the topic from Wes Smith, our Senior Vice President for Advisory and Consulting.
5. The industry has fully embraced value-based care.
The healthcare industry is fully committed to transitioning from an outdated fee-for-service model to value-based care. This is driving a major shift in population health management, as well.
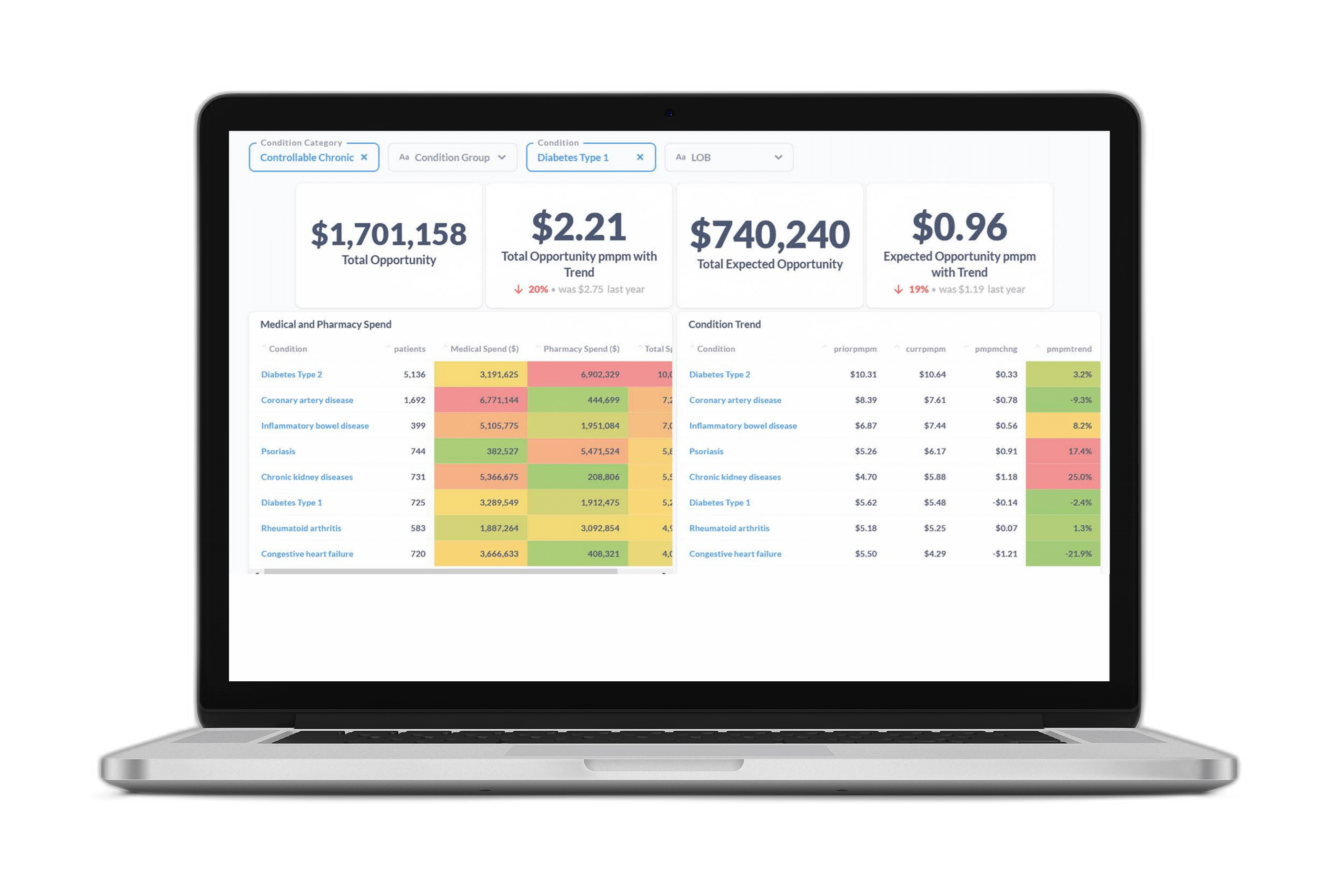
Traditional, retrospective analytic tools were built to serve the fee-for-service model—and they ignore the fact that the highest-cost members aren’t always the ones who will benefit most from clinical intervention. A member with lower overall financial risk—but more open care gaps or redirection opportunities—might be a better candidate for outreach, especially if the member shows a high propensity for engagement.
As healthcare organizations transition to value-based care, they’re moving toward prospective reporting that predicts not just risk, but modifiable risk, as we do through the Certilytics Opportunity Framework. This is the best way to reach members before they incur avoidable, exorbitant costs—and unlock true value while improving population health.
If you’re interested in learning more, contact us for a free consultation with our team of experts or see for yourself how we’ve helped healthcare organizations save $200 PMPY.