Despite the wealth of clinical and financial data available in the market today, predicting emerging High Cost Claimants (HCCs) continues to be a challenge. This is partly because few organizations have truly comprehensive historical data for every patient, employee, or health plan member. People change jobs, geographic locations, health systems, health plans – or all of those things at once – and they don’t necessarily bring their historical healthcare and benefits data along with them.
Even when significant historical data is available, there are often still gaps in the information.
Sometimes this is due to out-of-network care; other times, it’s because the person chooses to pay out-of-pocket for certain types of healthcare services or prescription drugs rather than using their medical or pharmacy benefits.
And of course, in many cases, the incomplete picture is due to disparate health IT systems that don’t play well together or can’t effectively reconcile conflicting information.
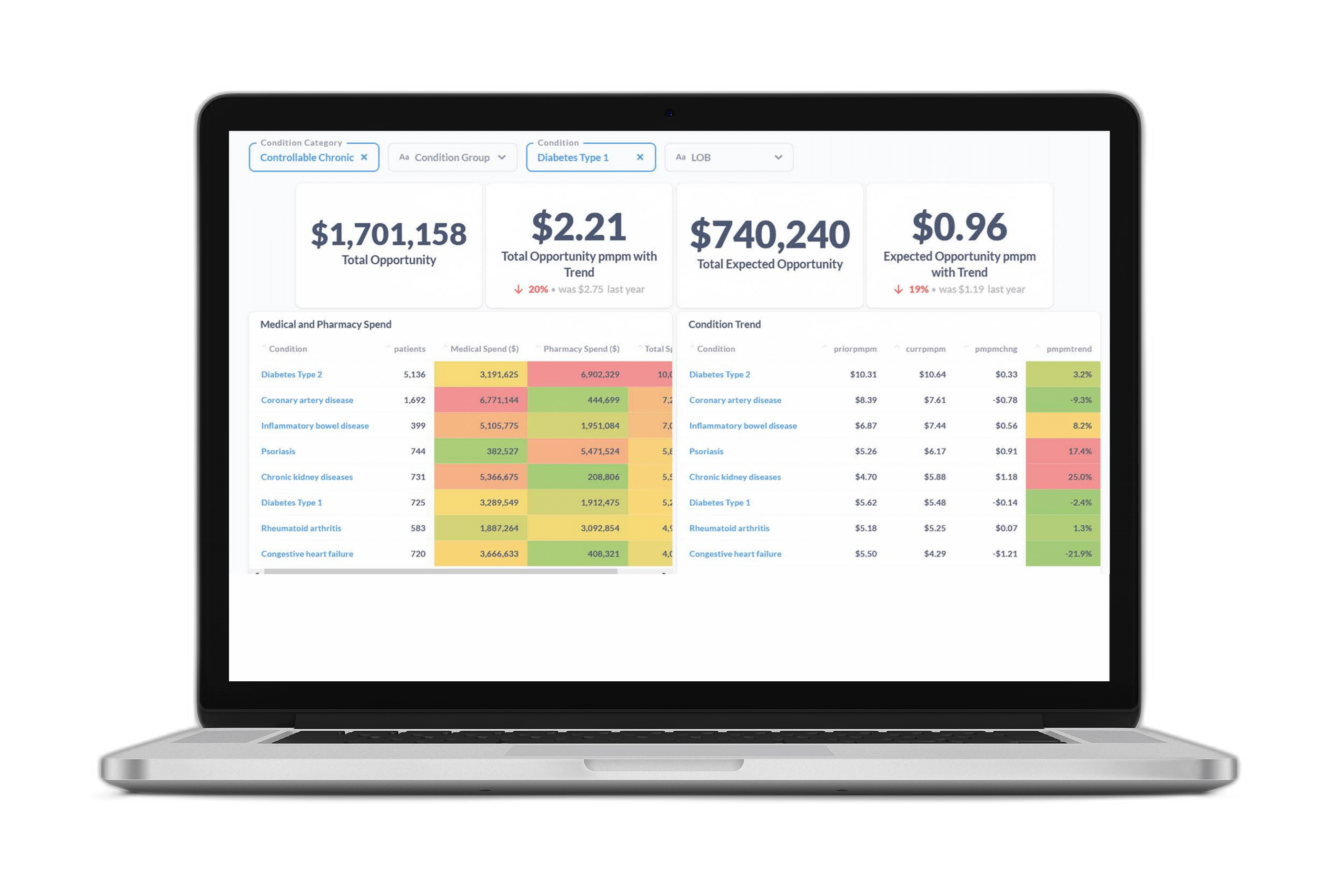
Whatever the cause, the result is that employers, health plans, and providers can’t count on having the data needed to predict those at risk of becoming HCCs using traditional methods. Accurate prediction of emerging HCCs enables earlier clinical interventions that can help a person better manage a chronic condition—leading to improved health outcomes and mitigating cost.
The challenge will only become more impactful as HCCs continue to become even higher cost – a clear trend line that will keep moving up and to the right thanks to innovative (and expensive) specialty drugs as well as the removal of annual and lifetime benefit limits under the Affordable Care Act.

A year’s worth of relevant data may also become even rarer in the wake of the COVID-19 pandemic. Forty-four percent of working Americans have plans to change jobs in 2021 alone. And although younger workers typically change jobs more frequently than older workers, in 2020 nearly ten percent of workers age 55-65+ had fewer than 12 months’ tenure with their current employer.
Improved Methods for Predicting High Cost Claimants
The good news? Advances in predictive modeling are helping organizations overcome the challenge of identifying emerging HCCs. Thanks to newfound ability to leverage non-traditional data sources and natural language processing technology that improves model performance when there’s limited patient/employee/member medical history, organizations are now able to accurately predict HCCs regardless of limited historical healthcare and benefits data.
In fact, these new models have achieved performance on par with several published models without the use of any member medical history – through a novel approach that infers health plan member risk based on the providers they’re seeing.