By Kelli Clark
Director of Sales, Employer Strategies
“Guess Who?” It’s a fun children’s game (and a fantastic Canadian rock band). But it shouldn’t be your approach when helping your clients design an effective employee benefits strategy.
And yet many advisors and consultants tell us they feel like they’re playing a guessing game when recommending health and wellness programs for their clients.
We’re here to help you stop playing “Guess Who?” and start playing … er, “Risk?” “Chess?” “Mahjong?”
Whatever your game of choice, here are three things we see our customers doing when they start taking a more strategic data-driven approach to how they evaluate health and wellness programs.
1. Start by connecting your clients’ data and taking a predictive analytics approach
Your clients are constantly being approached by vendors promising a new health and wellness program will be a game changer. They’re counting on you to help them make the best decision.
But, how do you know if these programs will truly meet the needs of your clients’ employees and their families?
It starts with connecting all your clients’ benefits data and analyzing it to see if a particular program will help solve the biggest health issues facing employees and their families.
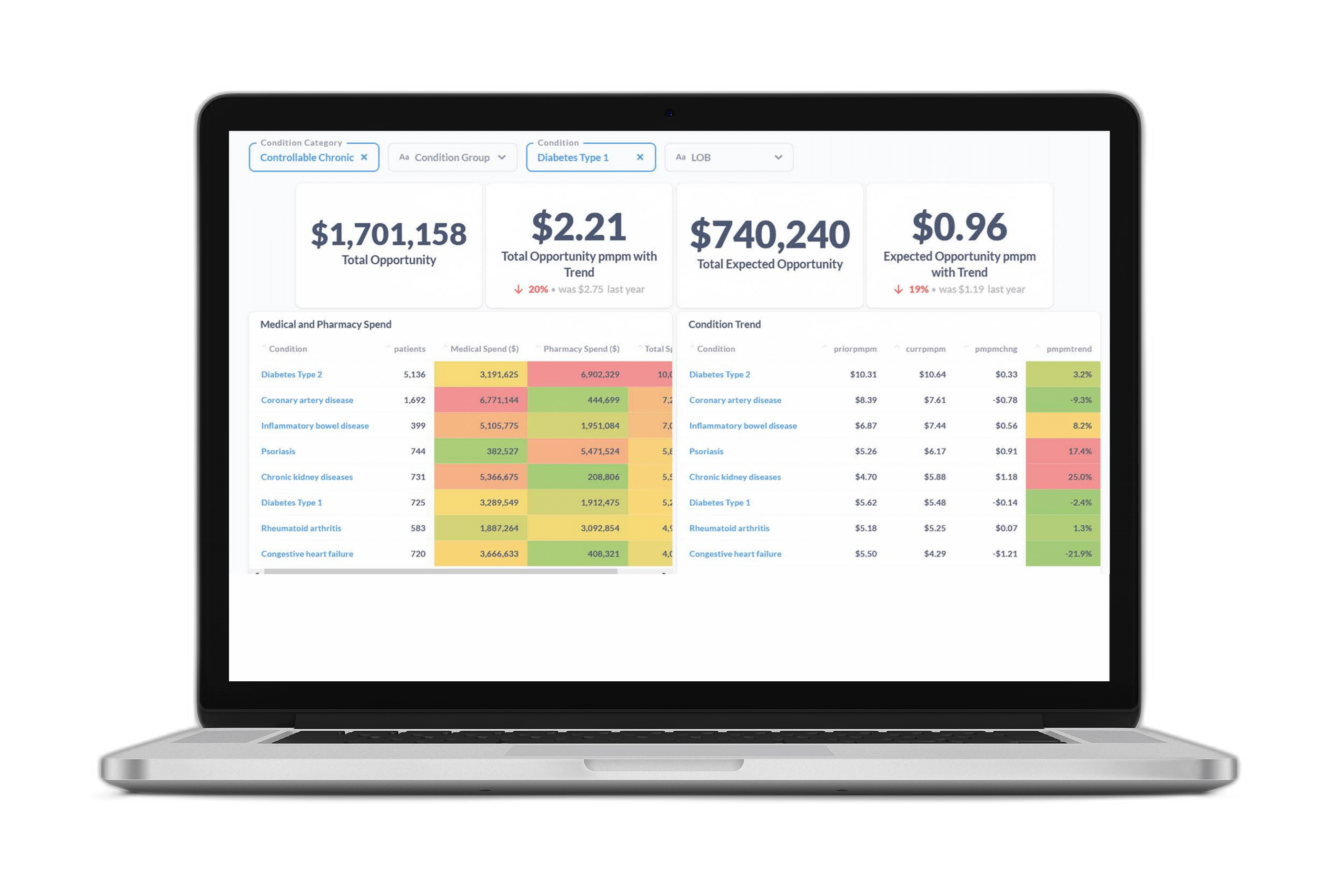
The first step is to connect all the data sources your clients have available (medical, pharmacy, dental, vision, wellness programs, etc.) using a comprehensive predictive data and analytics platform. This solution should be able tell you not just the prevalence of different conditions but also the areas with the largest opportunity to impact clinical and financial outcomes.
For instance, heart disease might be most prevalent and/or costly condition within a client population, but the data may show that employees with this condition are already extremely compliant and getting the preventive care they need. Diabetes may be less prevalent, but if those employees aren’t getting preventive care, it could make sense for your client to invest limited dollars in a diabetes management program rather than a heart disease program.
Here’s an example of the information benefits leaders we work with have access to when trying to determine the right solution:
2. Maximize program engagement with an AI-powered engagement strategy
“If you build it, they will come.” Have you ever helped a client put a program in place, but no one used it?
Lack of engagement is a frustration for many HR and benefits teams. Your clients want the time, money, and effort they’ve put in to selecting a new solution to help employees as intended. When employees don’t take advantage of a program, it can feel like a waste.
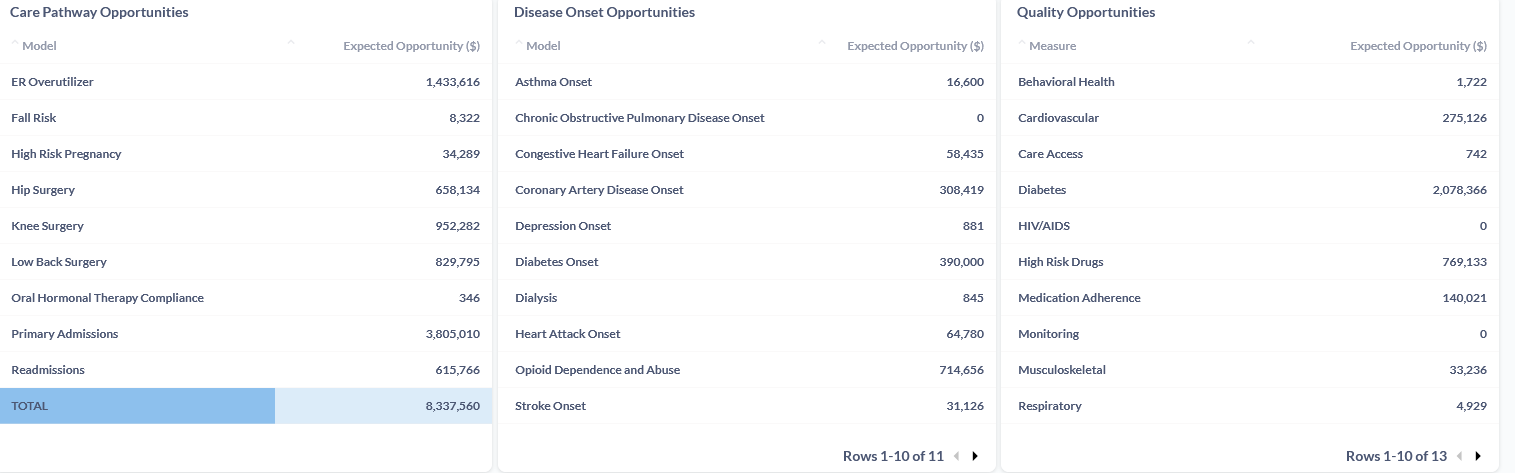
Benefits leaders are finding these answers by layering predictive analytics on top of their data, including AI-powered models for measuring each employee’s likelihood of engagement and the outreach methods they’re most likely to respond to. With this information, you and your clients will be able to work with vendors to direct outreach and education resources towards the employees most likely to benefit.
3. Have a plan for measuring program success
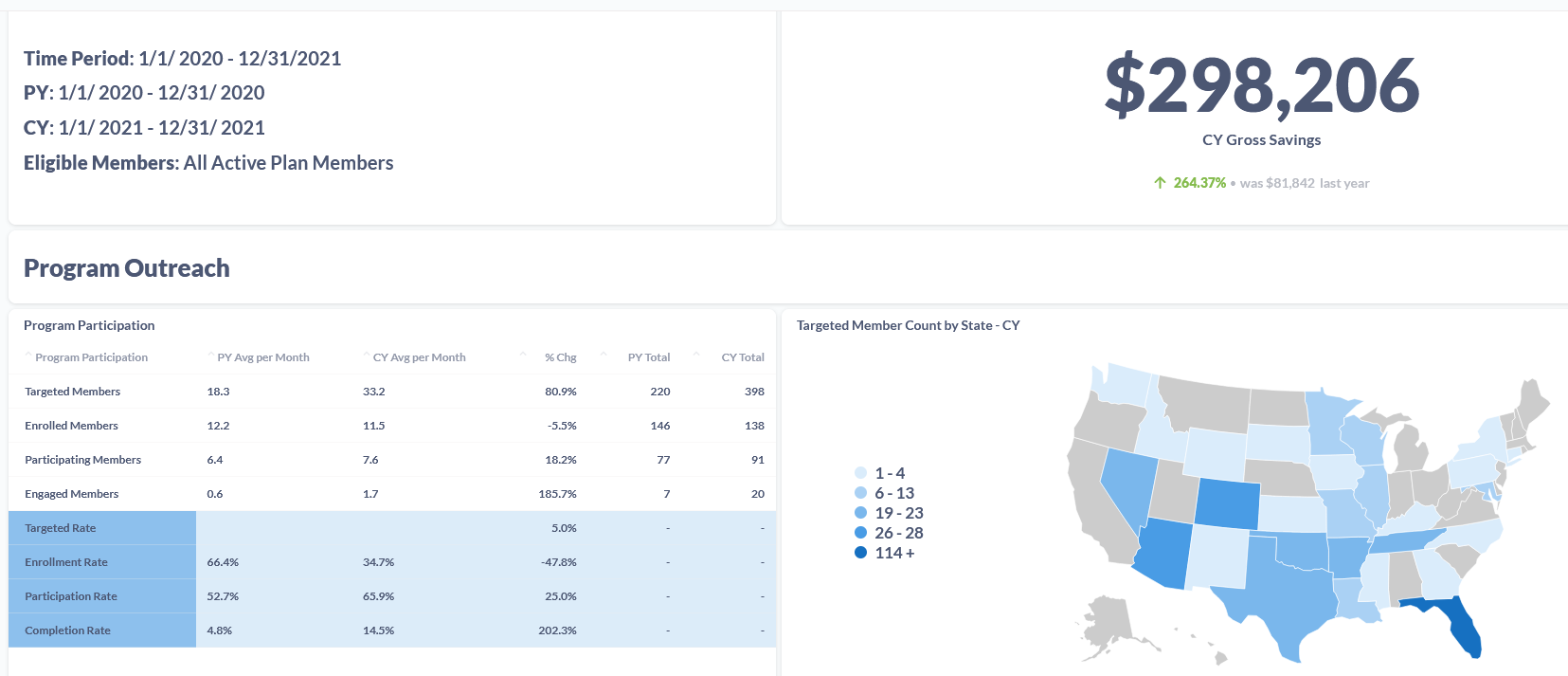
The return on investment from health and wellness programs is difficult to measure, given the number of variables involved. But advances in AI and machine learning are making it easier to quantify the impact of individual programs.
With data-backed program evaluation tools, you can determine what’s working for your clients’ employees, and what’s not —and build compelling value stories demonstrating your impact to clients.
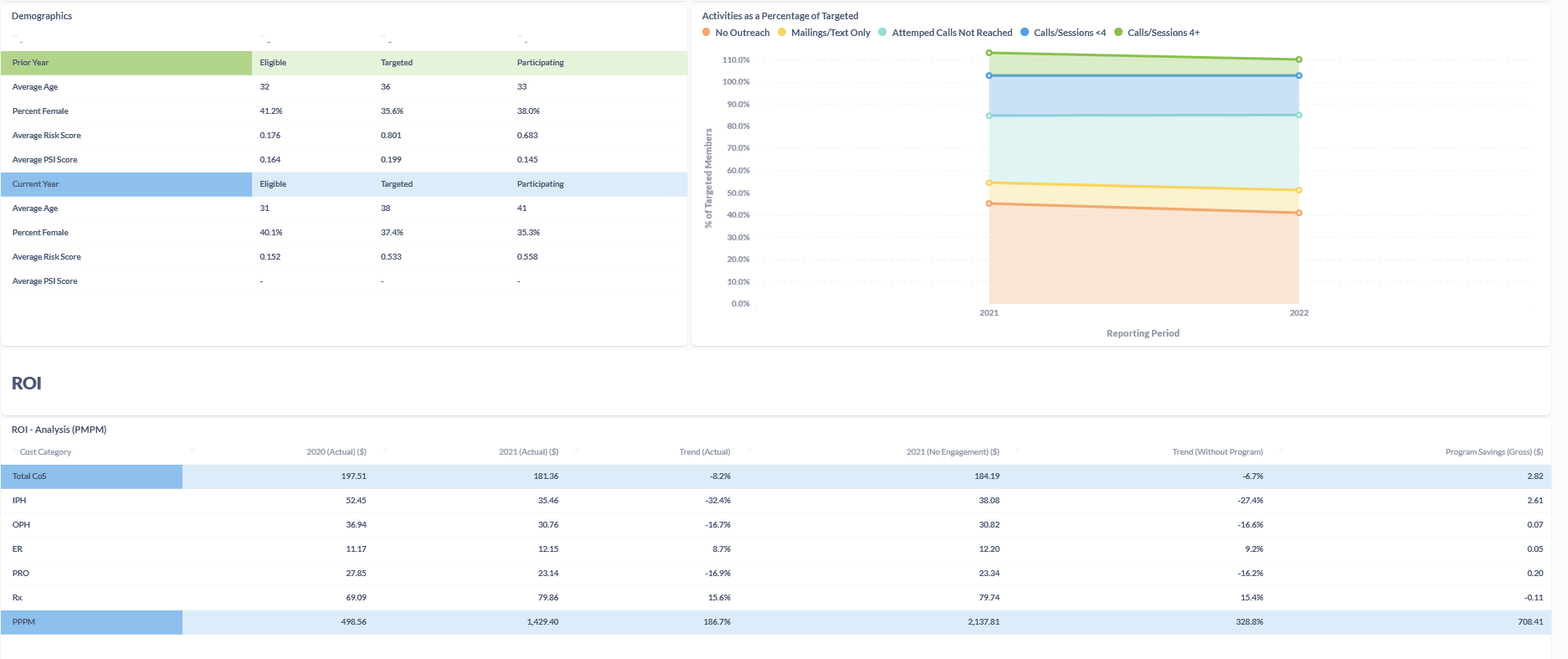
Here’s an example of the information benefits leaders we work with have access to through our Impact Evaluator program evaluation tool when trying to measure program success:
Are you ready to elevate your game on measuring the value and performance of your clients’ health and wellness programs?
Download our case study, or schedule a Q&A with our team.